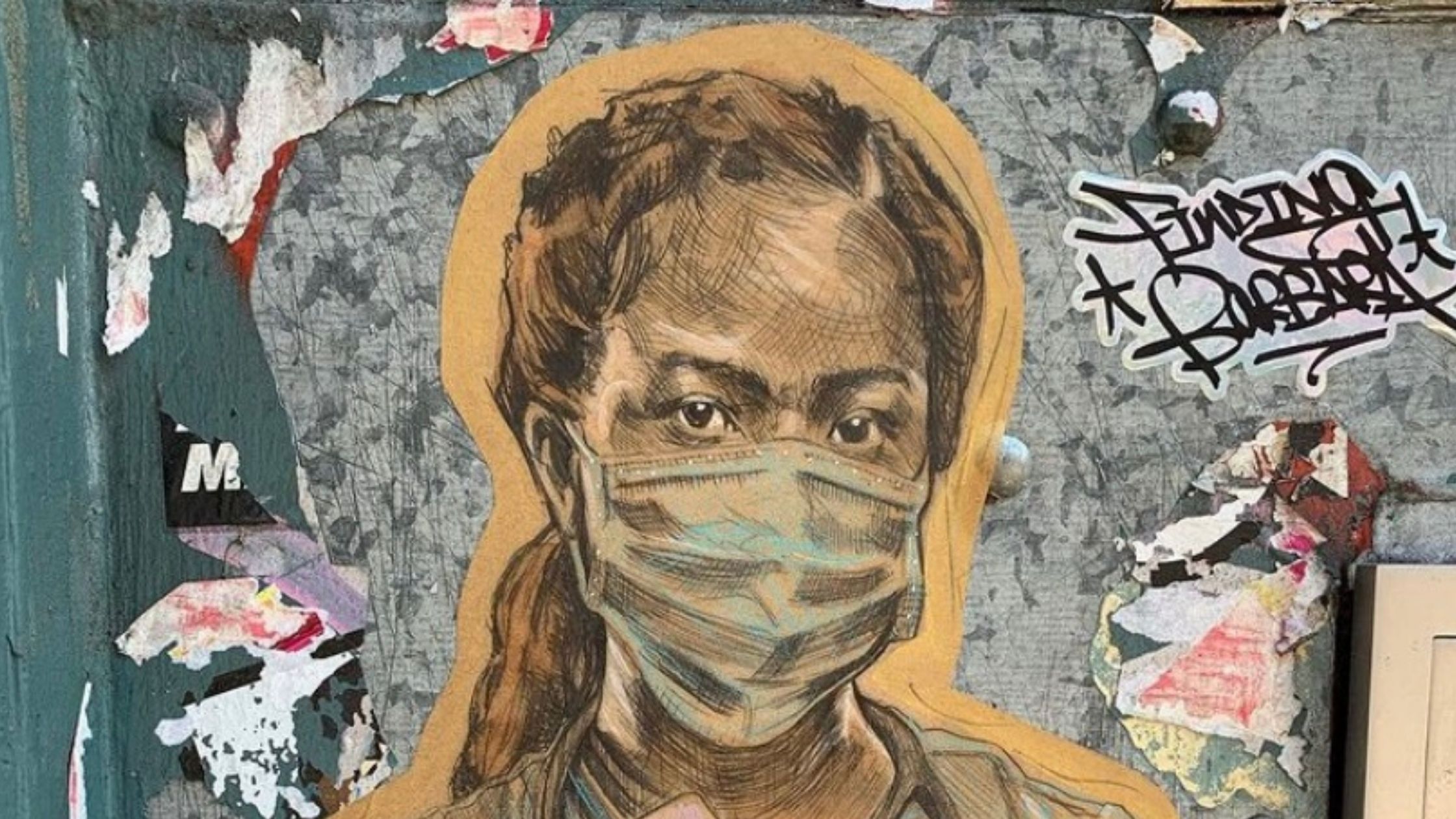
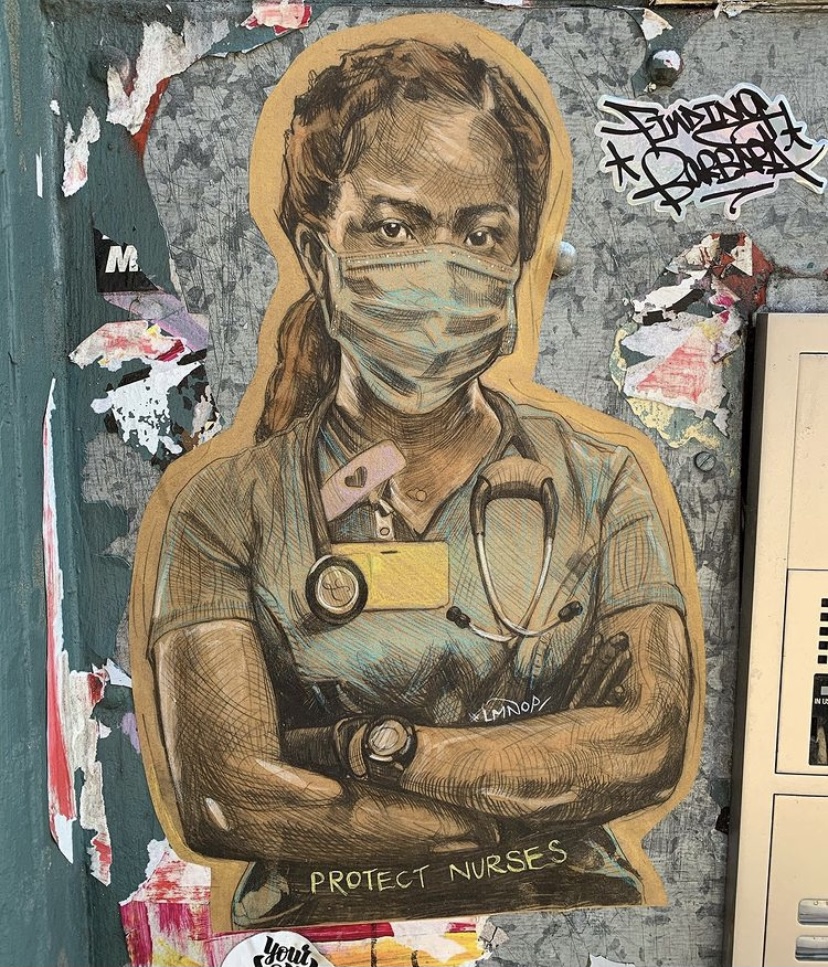
 COVID-19 rates are soaring nationwide, setting new records nearly every day. Recent reports show that doctors have learned a lot about how COVID operates in the past eight months – leading to briefer hospitalizations and fewer deaths. But as hospitals reach and then exceed capacity, doctors, nurses and other healthcare workers are again facing situations where resources are dangerously stretched.
COVID-19 rates are soaring nationwide, setting new records nearly every day. Recent reports show that doctors have learned a lot about how COVID operates in the past eight months – leading to briefer hospitalizations and fewer deaths. But as hospitals reach and then exceed capacity, doctors, nurses and other healthcare workers are again facing situations where resources are dangerously stretched.
These conditions can lead to moral injury, a form of psychological distress that results when someone’s actions, or inactions, violate their ethical code, or when they feel unprepared to face decisions or situations before them. Moral injury was originally described vis-a-vis the military: think soldiers on the front lines, forced to make decisions that will cause civilian casualties.
Moral injury is not, in itself, a mental illness, but it can contribute to PTSD, depression, or anxiety.
Today, our front line is the healthcare profession, and COVID has forced an ongoing stream of Sophie’s choices, where the options get more dire as the pandemic worsens. Which of two equally sick patients gets the last available ventilator? Who gets admitted first when there aren’t enough beds for everyone? When does saving the life of a milder COVID case trump using resources on a severe one when there aren’t enough supplies to do both? All doctors take an oath to avoid doing harm, and the pandemic’s strain on medical resources has made that vow difficult to uphold.
Moral injury is not, in itself, a mental illness, but it can contribute to PTSD, depression, or anxiety. And since doctors already have a suicide rate twice that of the general population – one doctor commits suicide every day in the US – it’s vital that hospitals prioritize helping their staffs process pandemic treatment experiences before, during, and after each COVID spike.
Today, our front line is the healthcare profession, and COVID has forced an ongoing stream of Sophie’s choices, where the options get more dire as the pandemic worsens.
According to a recent paper published in the British Medical Journal, psychological support is key for ensuring that what researchers called potentially morally injurious events (PMIEs) become a foundation for increased psychological resilience rather than a risk factor.
A few studies that have come out recently looking at healthcare workers during COVID-19 point to strategies for supporting them through the pandemic, including:
- Prepping healthcare workers for the moral quandaries they are going to face during the pandemic: We know that preparing staff for the job and its associated challenges reduces the risk of mental health problems later on.
- Checking in with staff who are “too busy” or routinely “not available” to process experiences in a group setting, since avoidance is a core symptom of unresolved trauma.
- Making time to reflect on the extraordinarily difficult experiences healthcare providers are facing to create a meaningful, rather than traumatic, narrative.
- Taking practical steps to manage anxiety, such as limiting time spent consuming news.
- Encouraging healthcare workers to seek support from trained peers and/or professionals when necessary.
Healthcare workers struggling with the hard emotional fallout of moral injury during COVID have the capacity to eventually experience post-traumatic growth…
It is important to note that most people who endure traumatic events like PMIEs will recover on their own and will not require professional support. Even most healthcare workers struggling with the hard emotional fallout of moral injury during COVID have the capacity to eventually experience “post-traumatic growth,” a strengthening of resilience, self-worth, and values after living through extraordinarily difficult circumstances. But making sure there are supports in place when healthcare workers need them will help ensure that PMIEs won’t contribute to wearing down exhausted front-line workers all the more.
The pandemic has dropped us all in largely uncharted waters, both medically and psychologically. But it’s becoming clear that current conditions, rife with potentially morally injurious events, are putting our healthcare providers at unprecedented risk. What we do know is how to help protect them, and it must become a top national priority.
About Us
At Center Psychology Group in New York, we specialize in providing compassionate and evidence-based therapy tailored to your unique needs. Whether you’re seeking EMDR therapy, Somatic Experiencing, or integrative trauma-informed psychotherapy, our experienced team is here to support you. Learn more about our services and how we can help you on the path to healing. Ready to take the next step in your healing journey? Book a free 15-minute phone consultation here.